37 patient safety events out of 436 sentinel events have occurred due to patient identification errors in the second quarter of 2019 including surgical or invasive procedure events involving wrong patient, wrong procedure, and wrong site.
A 2016 study classified over 7,600 out of 10,915 events from January 2013 to August 2015 as “wrong-patient events” involving patient identification.
That’s according to “Patient Identification Techniques Approaches, Implications, and Findings,” published in the National Library of Medicine.
Healthcare errors aren’t the only reason why medical patient registration is so important.
- Without proper medical patient registration, associating the individual with the treatment and testing they’re receiving, clinicians as many as 30% — may be forced to duplicate tests, increasing costs and decreasing patient satisfaction.
- Medical practitioners may create a second data record for the patient, creating more overhead for the practitioner, and running the risk that a healthcare worker might miss critical data that’s in only some of the records.
- Incomplete medical patient registration makes it more difficult for healthcare workers to share data and come to conclusions about more effective diagnoses and treatments in the population.
“Care decisions are based on an incomplete or erroneous picture of the patient’s medical history because data is not accurate or reliable,” warn authors of the paper.
In fact, the first of the “National Patient Safety Goals Effective January 2022 for the Hospital Program” by the Joint Commission is “Improve the accuracy of patient identification.”
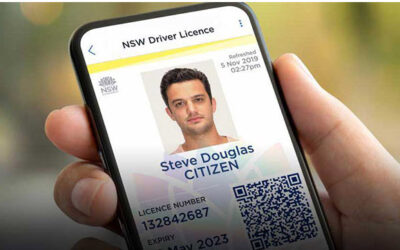
How healthcare workers use government-issued identification for medical patient registration
Technology is making correct medical patient registration even more critical, the paper’s authors write. “Ensuring quality health information has and will increasingly become complicated as new data streams are utilized and as organizations share records electronically using different information systems and standards,” the paper notes. But that’s more difficult in the United States than in other countries, because the U. S. prohibits the use of a national unique patient identifier due to privacy and security concerns.
Consequently, healthcare providers need to rely on identification documents provided by other organizations, such as national, state, and local government units.
Recommendations provided by the paper include “requiring patients’ photos to be taken at registration and incorporating them into patients’ medical records so that they are visible to all clinicians across the enterprise,” as well as “implementing standard processes for how staff should record certain patient demographic data attributes including patients’ names and addresses.” Government-issued identification documents often include both of these features.
For example, Safety Assurance Factors for EHR Resilience from the Office of the National Coordinator for Health Information Technology recommends that healthcare organizations requires a picture ID not only when verifying the identity of new patients, but also to authenticate the identity of established patients.
Why medical patient registration security is vital
At the same time, creating medical patient registration information creates a responsibility, both moral and legal, to protect that information and keep it safe.
That’s true in any industry, but it’s particularly true in healthcare, which operates under The Health Insurance Portability and Accountability Act of 1996 (HIPAA), a federal law that required the creation of national standards to protect sensitive patient health information from being disclosed without the patient’s consent or knowledge, according to the Centers for Disease Control and Prevention (CDC).
According to HIPAA, all covered entities which includes every healthcare provider, regardless of size of practice, that electronically transmits health information in connection with certain transactions, the CDC notes are required to:
- Ensure the confidentiality, integrity, and availability of all electronic protected health information (ePHI)
- Detect and safeguard against anticipated threats to the security of the information
- Protect against anticipated impermissible uses or disclosures that are not allowed by the rule
- Certify compliance by their workforce
“HIPAA violations may result in civil monetary or criminal penalties,” the CDC warns.
What makes the cloud the best place for storing medical patient registration information
Consequently, healthcare providers are increasingly moving their ePHI to the cloud, rather than keeping it on-premises. Storing data in the cloud is more physically secure, because it isn’t even stored on the healthcare site, and healthcare providers who are not necessarily information technology experts can rely on IT professionals to secure and back up their data.
Nowhere was this more true than during the COVID-19 pandemic, where organizations of all sorts including healthcare found that keeping their data in the cloud made it easier to pivot to supporting remote and location-independent work.
In general, a shift to the cloud will also accelerate innovation and improve customer satisfaction for healthcare providers, found Frost & Sullivan in its report, Impact of COVID-19 on Healthcare Contact Centers.
With medical errors considered the third leading cause of death, it’s more important than ever for healthcare providers to reduce the number of errors caused by incorrect medical patient registration identification.
Interested in learning how optical character recognition can help your business protect itself by using physical identification documents? For a free trial of our API or software, please email us at [email protected].